Beating The Opioids: How Cannabinoid Receptors Play A Key Role In Replacement Therapy
In the rush to beat the addiction and overdose crisis that’s not just hitting America, but killing people around the globe, many are turning to Cannabis as an answer. Both inhalation and ingestion of its extracts are particularly powerful in fighting the root cause of use, which is generally chronic or acute pain, either physical or emotional in the case of addiction. Many times our emotional pain will fuel our physical pain and vice versa. When it comes to the efficacy of using cannabis/extracts as a replacement for opioids, there’s a key element of science that’s beyond fascinating, the fact that all opioid receptors are literally engulfed in the trenches of CB-1 Cannabinoid receptors – the ones that really fire up when we inhale THC and are also ignited by the use of ingested cannabis from raw plant matter all the way to how CBD can tickle them via the various GPR’s (G Protein-Coupled Receptors like the GRP55). The science is simple on this one folk, cannabinoid receptors that get activated from the smoking, vaping, ingesting, dabbing, and other forms of intake of cannabis oils and products not only give us relief from our pain in many ways but also will cause the activation of those opioid receptors without using the pharmaceutical or illicit drugs that caused an addiction/dependence. It’s for this reason that we’re able to escape the probability that at some point the pharmaceutical drugs we take to help us will actually do us great harm.
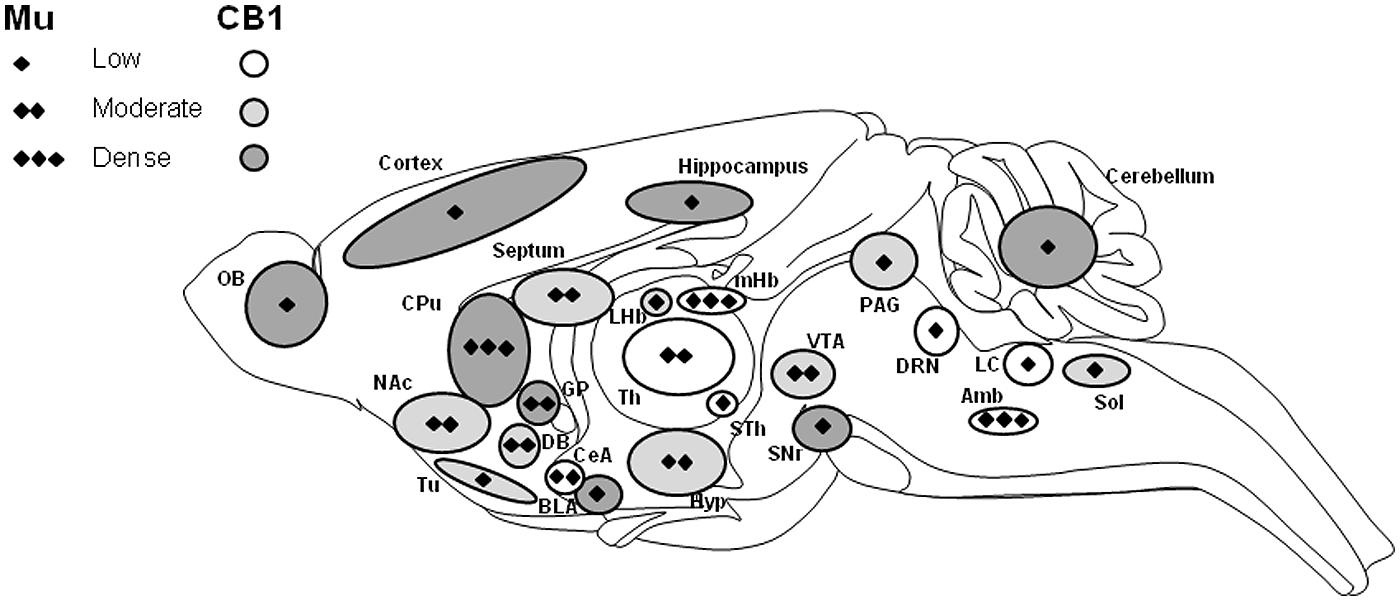
Above: “FIGURE 1. Schematic representation of the distribution of mu-opioid and CB1 cannabinoid receptors in the central nervous system. CB1 receptor distribution over the whole central nervous system is indicated by circle shapes with low (white), moderate (gray), and high (dark gray) expressions. Major localization of CB1 receptor (mRNA and protein) is in cortical areas, amygdala, striatum, and cerebellum. Moderate and low expression levels are observed in thalamic, hypothalamic, and brainstem regions. Interestingly, the mu-opioid receptor is also expressed in these CB1 expressing brain areas but at various levels, indicated by diamonds for low (one), moderate (two), and high (three) expression levels (adapted from Mackie, 2005; Erbs et al., 2014 and references therein). Amb, ambiguous nucleus; BLA, basolateral amygdala; CeA, central amygdala; CPu, caudate-putamen; DB, diagonal band; DRN, dorsal raphe nucleus; GP, globus pallidus; Hyp, hypothalamus; LC, locus coeruleus; LHb, lateral habenular nucleus; mHb, medial habenular nucleus; NAc, nucleus accumbens; OB, olfactory bulb; PAG, periaqueductal gray; SNr, substantia nigra pars reticulate; Sol, the nucleus of the solitary tract; STh, subthalamic nucleus (ventral thalamus); Th, dorsal thalamus; Tu, olfactory tubercle; VTA, ventral tegmental area.”
REVIEW ARTICLE Interactions of the opioid and cannabinoid systems in reward: Insights from knockout studies: https://doi.org/10.3389/fphar.2015.00006 CNRS, Laboratoire de Neurosciences Cognitives et Adaptatives – UMR7364, Faculté de Psychologie, Neuropôle de Strasbourg – Université de Strasbourg, Strasbourg, France
Introduction
Drug abuse often leads to a complex pharmaco-dependent state which is defined by the term addiction. Addiction is considered a neuropsychiatric disease. It develops from initial recreational drug use, evolves toward compulsive drug-seeking behavior and excessive drug-intake with the appearance of negative emotional states such as anxiety or irritability when the drug is not accessible, and uncontrolled intake reaching a stage where the drug interferes with daily activities, despite the emergence of adverse consequences (Leshner, 1997; Everitt and Robbins, 2005; Robinson and Berridge, 2008; Koob, 2009). This pathological process develops in 15–30% of casual drug users and several factors may explain an individual’s vulnerability to addiction, including genetic, psychological, and environmental factors (Swendsen and Le Moal, 2011; Belin and Deroche-Gamonet, 2012; Pattij and De Vries, 2013; Saunders and Robinson, 2013). Addiction is a major threat to public health and represents a societal problem especially in developed countries and the economic cost it entails (investments in research, treatment, and prevention) is considerable (Gustavsson et al., 2011). Read the balance at: https://www.frontiersin.org/articles/10.3389/fphar.2015.00006/full
Knowing this information allowed me to say enough, and end my own opioid crisis after 24 years. When I use Cannabis and its extracts it’s hitting the same areas of the brain necessary to curb addiction to pharmaceuticals – as well as for the illicit user. This information made me confident that I could say goodbye to the pills. Nearly 6 months after making that decision, daily it’s important to keep up on the cannabinoid medicine protocols I’ve established that definitely work. Using multiple delivery methods including inhalation, ingestion, and topical – I’m finally starting to feel like the “New Me” – as I don’t ever want to feel like the ‘old me’ again!
-Mike Robinson, Cannabis Patient and Founder, Global Cannabinoid Research Center. But, most of all, Genevieve’s Daddy
Sign up to receive informative and exciting email updates from Mike's Medicines!
You can sign up for our mail list here:
Didn't find what you are looking for?
Find exactly what you want to when you want it.
Browse through our archives by date, category or by entering a topic in the provided search field.
Archives
Categories
More to come as we have time to add them – there’s 100’s of additional publications!

We’ve made it easy for you to read Mike’s Medicine Blog or visit any of the Menu items right from here. It is that simple! Explore Mikes Medicines by clicking on the button below:
Read about how Cannabis Compassion and love created Mike’s beautiful family, the Cannabis Love Story inspires millions daily:
Genevieve’s Dream is all about her love for the Carousel coupled with her Cannabinoid Medicine journey – read more and make contact if you’re interested in collaborating with Mike!
The Global Cannabinoid Research Center is a trusted source for education, R&D, and more – make contact with us to collaborate.






